Then & Now
 I’d say it’s amazing how fast a year goes, but that’s so cliche. Instead, I will say that with my first-born, every day felt like a marathon. I felt like that newborn phase was going to last for the rest of my life. When I had my second, my perspective was much better. I knew it’d be a hard year and then it’d get easier.
I’d say it’s amazing how fast a year goes, but that’s so cliche. Instead, I will say that with my first-born, every day felt like a marathon. I felt like that newborn phase was going to last for the rest of my life. When I had my second, my perspective was much better. I knew it’d be a hard year and then it’d get easier.
Before I had kids, I couldn’t think more than a week ahead. I lived life day by day and rarely planned for anything and had a hard time committing to something unless it was going to happen the next day.
The days are long but the years are short, or so they say.
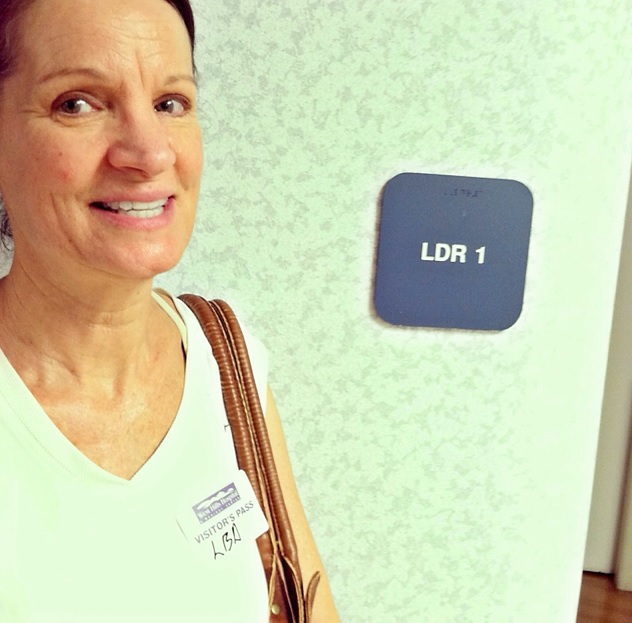
One year ago today I was sitting in the very same room as I type right now, in a birthing tub. This picture is obviously poor quality but it tells a story. The beginning of the story, anyway. A paper bag with a plastic bag in case I got nauseous (I didn’t), the sliver of the elbow of my midwife watching over me just barely making it in the right part of the frame, the birthing supplies in a trash bag on top of the pin ball machine that sat there un-used and taunting me for weeks (I was two weeks late), and Willy looking halfway helpful and halfway helpless.
I say it only tells the beginning of the story because we don’t have photos of the EMT’s who eventually came and had to transfer me butt-booty-naked in an ambulance to the hospital. We had our birthing plan all mapped out and, ultimately, we had to go with plan B.
Life doesn’t always go the way you plan it, does it?
And within ten minutes of being at the hospital, with one nurse pumping up and down on my stomach as if my heart were in my abdomen and I was in full cardiac arrest (clarification: I was not in cardiac arrest) and with some doc I had never met pulling and twisting, Van was born. All nine and half pounds of him.
On the days I work, I pump in a lactation room on the postpartum unit. I watched the other day as a newborn was wheeled past me and as I sat down to pump milk for Van, I thought how crazy it is that that little glow worm will be crawling and communicating and socializing in, what feels like, a blink of an eye.
Right now, Van is napping. I breastfed him while he held on to his blanket, his latest obsession, and laid him down in his crib. He quickly rolled over, hugging his blanket to his chest and sticking his little bum high up into the air.
One year. Three hundred and sixty five days. Fifty two weeks.
The days are long but the years are short; It’s true.
You can read Van’s entire birth story here.
Science vs. Technology
When I was pregnant with Hooper, my midwife palpated my belly. Her eyebrows raised and a look of surprise came over her face as she proclaimed, “he’s a long boy!”. Fast forward to his birth, where he measured 23 inches. She nailed it, he was a long boy. And that’s just one of many things I love about midwives; they use and trust their hands.
When I went to see my new backup OB, he confessed that he cannot tell the difference between a babies rump and head when he is palpating a woman’s pregnant belly. He also confessed that although he wears one of the most expensive stethoscopes around his neck, he hardly ever uses it and cannot tell the difference in various heart rhythms. Instead, he said, he relies on ultrasound for detecting the baby’s position and an EKG to determine heart rhythm. He’s young and he’s the product of modern day machinery, I mean medicine.
At any rate I recently read a fascinating article, “The Most Scientific Birth Is Often the Least Technological Birth”, written by Alice Dreger, a professor of clinical medical humanities and bioethics at Northwestern University’s Feinberg School of Medicine. She starts the article by sharing the answer she received when asking her medical students what came to mind when they envisioned someone who chose a midwife over an obstetrician. The students described a granola girl. You know, they one’s that look almost Amish and frolic in fields of grass and mix herbs from their gardens in their spare time.
I don’t consider myself a granola girl at all, in fact, I’m slightly offended when someone refers to me as a “hippie” because I’m choosing a home birth. Instead, I consider myself very rational. I also find myself to be a hostage of my own principles. It’s nearly impossible for me to do something I don’t believe in. And I do believe in medicine, otherwise I would not work at a large hospital as a registered nurse. But I believe their is a time and place for medical intervention.
Dreger goes on to make a clear differentiation between science and technology, noting that the scientific literature shows that interventions used during birth actually increase the risk to mother and child instead of decreasing it. A bold statement made by someone both in the academic and medical worlds, no? She states the problem with her medical students is that they think that what it means to be a scientific doctor is to bring to bear the maximum amount of technology on any given patient. And this, she says, makes them dangerous.
It goes without saying that all woman want a healthy outcome when it comes to birthing their child. The problem today, she says, is that no one seems to tell them what the data indicates is the best way to get there.
Recounting her own pregnancy in 2000, she says:
“My mate and I consulted the scientific medical literature to find out how to maximize safety for me and our child, here’s what we learned from the studies available: I should walk a lot during my pregnancy, and also walk around during my labor; doing so would decrease labor time and pain. During pregnancy, I should get regular check-ups of my weight, urine, blood pressure, and belly growth, but should avoid vaginal exams. I should not bother with a prenatal sonogram if my pregnancy continued to be low-risk, because doing so would be extremely unlikely to improve my or my baby’s health, and could well result in further tests that increased risk to us without benefit.
According to the best studies available, when it came time to birth at the end of my low-risk pregnancy, I should not have induction, nor an episiotomy, nor continuous monitoring of the baby’s heartbeat during labor, nor pain medications, and definitely not a c-section. I should give birth in the squatting position, and I should have a doula — a professional labor support person to talk to me throughout the birth. (Studies show that doulas are astonishingly effective at lowering risk, so good that one obstetrician has quipped that if doulas were a drug, it would be illegal not to give one to every pregnant woman.)”
Drawing from several experts in the birth world, Dreger points to the problem in the way birth is conceived in America — as “dangerous, risky, and in need of control to ensure a good outcome.” She also touches on the lack of insurance coverage for births outside of the hospital setting, the misuse of science to support the new technologies of birth, the lack of information provided to woman regarding the dangers in interventions offered, and the limited options women in America have in regards to bringing their child into the world.
I had to fight hard for home birth coverage. I wasn’t even aware that coverage could have been obtained the first time around and thus had to pay out of pocket for something that in hindsight could have been covered had I had more knowledge or had someone presented my options to me. Instead, obtaining home birth coverage was something I did proactively. I made home birth an option for myself, no one presented it on a silver platter. It’s unfortunate because I know a lot of women don’t have the time or energy that I did to put toward it, even if our desires for the best birthing outcome are the same.
Dreger concludes by stating, “We’re all very interested in having healthy babies and it is pretty easy to make the kind of cognitive errors that people make, and attribute to technology benefits that don’t exist. At the same time, when there are problems in a pregnancy, that very same technology can be life-saving. It is easy to make the [problematic mental] leap that technology is always going to be necessary for a good outcome.”
I get that this is a touchy subject. You can check out the comments to her article if you really want to get fired up one way or the other. I get that a home birth is not for everyone. I get that a natural birth is not for everyone. I get that some women are more comfortable birthing in the hospital setting and I get that some prefer an Obstetrician to a Midwife. But my bottom line has never wavered: Women need to be educated. The consequences of many of the interventions throughout labor need to be discussed and options need to be more available.
What are your thoughts on the topic?
You can view the whole article here.
Photo Source.
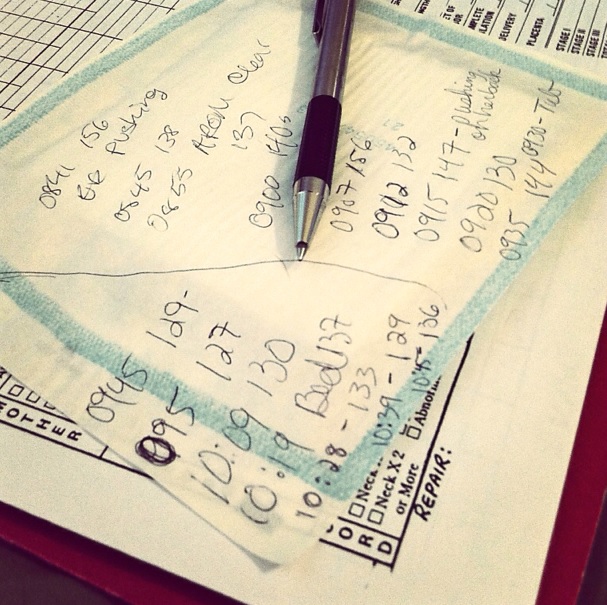
Steps to Obtain Insurance Coverage for a Home Birth
1. Speak with different midwives in the area. All the midwives I spoke to seemed to offer different types of advice for getting insurance coverage and were extremely helpful and hopeful. Ask your midwife for specific information like their license number, EIN and NPI number, and even the CPT code. These are all helpful to have on hand and eventually necessary when finally getting through to your insurance company.
2. Call the member services 800 number on your insurance card and explore exactly what your benefits are.
3. Get transferred to the medical management department and explain that you are in need of pre-authorization or pre-certification for midwife services.
sidenote: It is my understanding that all midwifery care is considered out-of-network. In other words, no midwives operate as in-network providers. This does not, however, mean that they won’t cover it. It simply means that they need to agree to cover it before they are billed for such services in order to guarantee payment.
4. Get connected with a nurse case manager. This person is your best friend. Be nice, but be painfully persistant. This person is the one that actually applies for the pre-certification. You want this person on your team. This person will also be in close contact with your midwife, as they need information from both ends to make it all happen.
5. Your nurse case manager will initially try to explain that you need to stick to in-network providers. They will do their own search of in-network midwifery services and tell you to start with that list of providers first. My case manager prompted me to search through what she described as “2 pages of in-network providers”. When I ran the same search, there certainly were two pages. All the providers had the same address and phone number, however. When I called, they explained that they worked out of a hospital in downtown Los Angeles and did not offer home birth services. For those that are familiar with the LA area, you know that trying to get to downtown LA, depending on the time of day, could be insane. Especially for a laboring woman. This prompts the next step…
6. Explain why their list of in-network providers will not work. I explained that not only do they not offer the care I’m looking for, but that I’d also run the risk of delivering on the side of the road as navigating through LA traffic while in active labor wasn’t the safest plan. They will then proceed with obtaining what they call “in for out” coverage or in-network benefits for out-of-network providers.
7. Call daily for updates.
8. Obtain your pre-authorization number.
Wow, I can’t believe it can all be summed up in 8 steps. The entire process took about a week. Here are some additional tips I had found in my research:
-Keep notes of dates, times, people, and departments that you speak with.
-If you feel like you are coming up against a bump in the road, explain that you are trying to save them money. If the person you are talking to doesn’t seem thankful for the fact that a home birth is much more affordable for the insurance company than a hospital birth, then ask to speak to their supervisor. If the supervisor is a carbon copy of the idiot you were just speaking with, ask to speak to their manager. Eventually you will speak with someone who appreciates the save in cost.
-If they deny the pre-authorization, ask for details regarding the appeal process. I fortunately know nothing about this process other than it exists and others have successfully appealed, so if you are in this position, do not give up!
Here are three links I found useful in my research: one, two, three
…And now, some inspirational birthing images:
Photo sources: 1, 2, 3
16 Weeks
What was a battle last week has already ended in celebration this week. I have to say, I was quite prepared to go the distance. I had already researched the appeal process. I have notes with dates and names of people I talked too, all neatly kept in anticipation of having to include them in my appeal letter. Why am I celebrating, you ask?
Because I have an authorization number. From my insurance company.
What’s an authorization number, you ask? Oh, it’s just a little series of numbers that represent approval. Approval of a home birth. Yup, approval to cover the fiances of our home birth.
Hip hip hooray. Hip hip hooray. Hip hip hooray.
Wanna know how I did it? I’m dying to share. Stay tuned…
An Update
Lucky for us, our midwives have a couple OB/GYN’s that back them up, so to say. This, in and of itself, says a lot about not only what they do but how they do it. I definitely have my issues regarding trust of the mainstream medical field when it comes to labor, but seeing an OB that I know my midwives trust helps soothe some of my anxiety.
Since our appointment with our midwives, I’ve done a lot of reflection regarding what’s important to me and what I feel is best for myself, this pregnancy, and this baby. Keeping to my New Year’s resolution, I reached out to positive, educated, and encouraging individuals and what I got in return was just the support I needed.
I had one friend from High School that put me in contact with her sister-in-law who has had a home birth and is preparing for her second, also to be born at home, in March. She shared a story with me of a friend that also planned a home birth, labored at home for 22 hours, and ultimately transferred to the hospital where she underwent a medically-necessary c-section. It happens. It was her perspective that I found enlightening. She said: medical intervention helped her in the end, laboring at home helped her in the beginning. This same friend went on to have her second baby at home, in a pool in her living room, with no complications.
Always up for a good debate, I like to play the devil’s advocate. I sent an email to our OB, Dr. K, who delivered Hooper on the operating room table. Here’s what he had to say:
As we talked about in the office, I think your odds of an uncomplicated delivery are extremely high. Second labors tend to be faster and easier than first labors and less second pregnancies go past the due date. I do not, however, have a crystal ball and there are certainly patients attempting home births who need to be transferred in labor due to some issues that arise. I do not think your chances are any higher than anyone else just because of your first labor. I do back up midwives because I think it important that patients have options and choices. I am also very up front if I think that choices should be limited because of circumstances. I see no such issues with your pregnancy at this point. My agreement with the midwives that I back is that I will agree to care for patients that they feel are no longer low risk. I obviously do not tell my patients to seek midwife care but I would always agree to back them if that is what they chose. You have become my patient and I would always try to give you advice that keeps you in the realm of safety while trying to allow you to ‘get what you want’. I think you are an excellent candidate for a home birth if that is your choice. If you choose that, I will be happy to serve as your back-up MD in case there are issues that require my attention or your transport. I hope this helps you.
And help me it did.
With Willy on board as much as he’s gonna be on board and with the support I so desperately needed, I’m feeling good. I feel more confident than ever about my decision.
A special thanks all those who have reached out to show their support, espically to Ali for putting me in touch with Abby, to Dr. K, to Janet for listening to me vent when things needed to roll off my chest, to my midwives whose patience, support, and love for what they do seems otherworldly, and to my lovely husband who listens to all my crazy shenanigans and trusts me enough to join me on this journey. Willy, you are the crispy pickle to my sandwich. Oh gosh, now I want a pickle. A really crispy pickle.
Photo credits: source 1, source 2
More Business of Being Born
Have you heard of the Ricki Lake and Abby Epstein’s Documentary, “The Business of being born”?
Well there is a sequel. I ordered it today. You can watch the trailer below and if you find the girl in the middle of the group at the end incredibly annoying, you’re not alone. Otherwise, can’t WAIT to see. Thank you to Ricki Lake and Abby Epstein for making such an important cause mainstream.
If you’ve seen either of these documentaries, what were your thoughts?
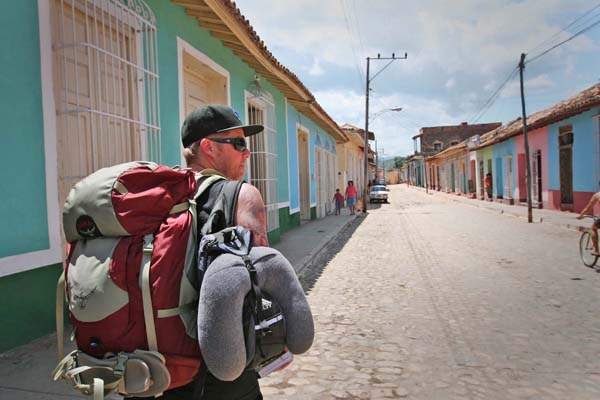
Infant Mortality Rate
Have you ever looked up infant mortality rate in the United States? The results are shocking. You’ll find yourself scrolling further than you think to find the US’s home on the list. According to the CIA’s world factbook, we are ranked 48th in 2011, behind Cuba. Behind Cuba, people!
Willy and I visited Cuba in 2010.
We travelled there legally with humanitarian licenses. Ironically enough, we were responsible for bringing medical supplies to a mission in Havana. Ironically, these supplies included things like prenatal vitamins. Yes, you are understanding me correctly. We, US citizens, supplied Cuba with prenatal vitamins. Yes, Cuba’s infant mortality rate is lower than the infant mortality rate in the US. Interesting, no?
The other day we met with a realtor to discuss the option of selling our home. We mentioned Zillow in the conversation and the guy rolled his eyes. This was the second realtor we talked to that rolled their eyes upon mentioning Zillow. So we questioned the eye roll and his response was something along the line of too much information being provided to people that are not educated enough to filter it correctly. Information overload.
Back to the infant mortality rate.
The rate of medical intervention in the US is presumably higher than the rate in Cuba. Would anyone argue against this? I think birth in the US has become too medical. I think there are more interventions because there is more monitoring. This sounds like a crazy statement, I know. But there’s been lots of research done to support this claim. The following excerpt was taken from an interview with Dr. Alex Friedman:
There are numerous reasons that one of three U.S. births now is by cesarean, but Dr. Alex Friedman blames some on an imprecise monitor strapped to laboring women. Too often, he has sliced open a mother’s abdomen fearing the worst, only to pull out a pink, screaming bundle.
“Everyone knows it’s a bad test,” said Friedman of the Hospital of the University of Pennsylvania. “You haven’t done the patient a big service by doing an unnecessary surgery.”
Electronic fetal monitors record changes in the baby’s heart rate, a possible sign of too little oxygen. They became a tradition — now used in 85 percent of births — years before research could prove how well they work.
Guidelines issued last summer, aiming to help doctors better interpret which tests are worrisome, acknowledge the monitors haven’t reduced deaths or cerebral palsy. But they do increase the chances of a C-section. While they should be used in high-risk women, the guidelines say the low-risk could fare as well if a nurse regularly checked the baby’s heart rate.
Information overload.
In looking at the US infant mortality rate versus Cuba, I do think it is only fair to look at the counter argument. Because we have more medical technology the number of high risk babies born is higher in the US. I found the following information here.
In the United States if an infant is born weighing only 400 grams and not breathing, a doctor will likely spend lot of time and money trying to revive that infant. If the infant does not survive — and the mortality rate for such infants is in excess of 50 percent — that sequence of events will be recorded as a live birth and then a death. In many countries, however, (including many European countries) such severe medical intervention would not be attempted and, moreover, regardless of whether or not it was, this would be recorded as a fetal death rather than a live birth. That unfortunate infant would never show up in infant mortality statistics.
In any event, when I research birth I look for information as it relates to me. If I happen to go into preterm labor at 20 weeks, my midwives will certainly not support or participate in a home birth. I would be in the hospital kissing the fetal monitor and thanking the doctor for any interventions that could potentially save my baby. But if my pregnancy remains low risk and if I remain healthy, I feel strongly that delivering at home is safest for me and, perhaps more importantly, for my baby.