A while ago, I posted here and on instagram about my own personal experiences with midwives and compared it to my current experience with my OB. While many commented and shared similar sentiments, there were still others who defended their own positive experiences with their OBs (and hey, more power to them). If there ever was an asterisk attached to anything and everything I share, it would read this: *based only on personal experience. I’m hardly trying to be the voice for anyone other than myself. It’s hard enough at times to find my own voice, I certainly don’t feel the need to put words in the mouths of others.
One reader, however, caught my attention. What she said was not judgmental or harsh, but rather she expressed sadness with the way OBs are bashed. She said, “There are many practices out there, like my own, where its a collaboration between midwives and OBs – we both benefit from each other and most importantly the patient benefits… The focus on birth and birthing stories, birthing photography, videos, etc has sadly turned such a private intimate moment for a family into a business and a chance to out do each other… Birthing is one of the most sacred moments in a woman’s life, but it’s only one moment of many to come for the couplet”.
I use my blog to share my own experiences, sure, and whoever follows along can follow along on their own free will. But when given the opportunity to expand and share a different side of the coin, you better believe I’m grateful. I realize that my own experiences are a mere drop of water in the ocean and anytime the opportunity should present itself to share a different point of view, I’m all about it.
So, I contacted Ema and asked her if she’d be willing to share more about her OB practice and thoughts, in general, about the current state of birth. I feel so fortunate to have her and hope you all can appreciate the conversation; because that’s what it’s all about — not who’s right or wrong, but the dialogue.
For the past 8 years, Ema has chosen to work in OBGYN-Midwife collaborative group at North County Health Services, where they have 5 OBGYN’s and 10-12 Certified Nurse Midwives (CNM). With no further adieu, here’s Ema…
It could easily be argued that the way you have designed your practice is quite progressive, as the tandem approach to patient care between OBs and midwives is not something we see often. Why have you chosen this model and what would you say the advantages are?
I am certainly blessed to have found North County Health Services. But in reality, I think it actually found me. My entire training starting in residency has been along side midwives. I did my residency in the military, an institution that is very progressive in its use of ancillary health professionals, specially midwives. The biggest advantage I see is that it is a win-win for the patient. As one of my OBGYN colleagues jokingly says, “they do all the crunchy-granola stuff and we do the high risk stuff”. But it is all part of the same practice. Patients get the sense that there is a team based approach to their care, multiple eyes reviewing their antepartum care, if complications arise, the OBGYN is a phone call away and if all goes well, the patient receives a hospital based midwife attended delivery.
The advantage is that it is the best of both practice patterns. The key to our practice is that it is truly collaborative- we all meet for 4 hours weekly to discuss cases, learn each others’ practice patterns, and share info/management plans on the higher risk patients. This helps bridge the gap in communication and overtime reinforces the trust needed to have this unique collaborative model.
In recent years, there has been several documentaries put out about birth. Take the Business of Being Born, for example. Have you seen it and what are your thoughts on it?
Indeed! There are in fact several documentaries. I have watched Business of Being Born. Although this movie was revolutionary in highlighting the natural and gentler side of child birth (providing contrast to the mass media depiction of a screaming birth), what it did do is provide a very biased depiction of this business.
The OBGYNs that were in the movie seemed to be unfamiliar with natural birth options and hence the debate started off with an unfair advantage. I read in an article while researching this answer, “Noam Chomsky once pointed out that if you only allow two view points, and then allow vigorous debate between the two view points, you can achieve the appearance of democracy and free speech without ever actually having it.” What I do appreciate about the movie is that it is a good starting point for further discussion. For example, although the profession of “midwife” or “midwifery” is used in this film, it should be noted that there are several types of midwives. Lay midwives, certified midwives, and certified nurse midwives- which are the only ones who can work in a hospital setting. They have far more extensive training and education than lay midwives. The audience is left to think that there is only one kind of midwife practice without any indication that there are vast differences between these subsets.
I think these documentaries are somewhat responsible for a certain degree of fear some women have toward birthing in a hospital. Would you agree? Do you think this fear is justified?
Once again by the biased portray of the business of midwifery vs. obstetrics, yes, movies like BOBB, feed the fear in the masses. As I mentioned before there are a plethora of documentaries on birth that I would recommend:
1. Birth Story: Ina May Gaskin and The Farm Midwives
2. Midwife
3. From Conception to Birth
4. BBC documentary Childbirth All or Nothing
In addition, there is a great website that we encourage moms to look at: www.evidencebasedbirth.com
I had horrible side effects following induction via Pitocin. I’ve read that Pitocin, while FDA approved for the induction of labor is not actually FDA approved for the augmentation of labor. Can you discuss the validity of this?
Regarding pitocin- Pitocin is the brand name of the synthetic form of a naturally produced hormone called oxytocin. It is derived from the pituitary gland of mammals. According to the FDA or look on the FDA or other resources such as Physician Desk Reference, or websites such as drugs.com or rxlist.com, Pitocin is indicated for the initiation (induction) or improvement (augmentation) of uterine contractions.
Therefore, I am not sure about the validity of the statement that it is not FDA approved for labor augmentation.
That being said, Pitocin is a drug and like any other drug it does have negative side effects. Some of the reported reactions include: anaphylaxis, nausea, premature ventricular contractions, hypertensive episodes, and with high doses uterine hypertonic its, spasm, or rupture of the uterus. Therefore, beyond a certain limit, pitocin needs to be administered with an intrauterine pressure catheter.
There is a presumption that some OBs prefer performing a c-section to a natural birth for selfish reasons: more money, easy to schedule, etc. Have you noticed a trend of this sort among your colleagues? Can you speak to how the decision for some to go this route may taint the perception of the field of obstetrics as a whole?
I think this is similar to the “bad apple” question. I would like to think that I work in field with other altruistic physicians whom also have taken an oath to do no harm. Therefore, even though there might be some who shift the pendulum, I firmly believe that these practices of financial gains and convenience are outliers and certainly not the norm. And therefore, I am incredibly saddened that the few have tainted the perception of the many. But I do hope that with conversations like this and continuous open discussion we can help shift this biased view.
I have two young children and a very busy schedule. We’re new to the area that we live and this will be my first birth in this new area. What tips would you recommend to someone like myself for finding a good fit in an OB without having to waste time I don’t have interviewing several? And what kinds of questions or things should one ask or look for when searching for an OB? As I touched on in my initial post, the OB I see was recommended to me by the local birth center, which was a huge deciding factor for me. It is also important that he is a sole practitioner as I mentioned that many of the OB practices in my area are part of a larger medical group and that continuity of care within these medical groups is typically lacking.
I think what you did is exactly perfect. Reach out to your local birthing center and ask for references or the names of their back up doctors. Generally, but not always, these physicians have experience with midwifery care and can appreciate the different approaches. You do need to interview, there is nothing, no Yelp, for physicians that would beat the actual gut feeling when you meet a physician. I would encourage women to ask A LOT of questions regarding the relationship between the midwives and the supporting physicians. One key factor is the financial drive in the relationship. For example- if a group of midwives is working with a group of physicians and the midwife refers a patient to the physician for a consult, it would be financially advantageous for the physician to “label” this patient as high risk and therefore take the patient for him/herself. This would then create a distrusting relationship between the two groups and ultimately put the patients at risk. The midwives would fear loosing their patients and would be less inclined to refer or consult. Therefore, a true collaborative model where there is no financial incentive between the parties is the model that works best.
Because you’re passionate about what you do, does it bother you that a few bad apples have more-or-less tainted the overall impressions of OBs? I’m sure reading experiences like mine weighs heavy on your heart and I wonder if you can’t see how other OBs have essentially worked against the fight you are fighting? And if I’m wrong on this entirely, feel free to call me out. I understand this statement may boarder on being presumptuous.
Of course, in all professions however, there are always outliers. The key here is to not be swayed by the “bad apples” and media and continue to do what at the end of the day is good medicine. There is an art to medicine and that is one of the reasons I truly love my job. Unfortunately, “bad apples” lead to stricter guidelines that ultimately end up in the loss of this art. It is a continuous battle.
You clearly see the benefit of utilizing midwives as they are, in your own words, “the first responders” in your practice. Why don’t you think more midwives are used within the hospital / obstetrics settings?
To answer this question you need to recognize that the term midwife is an umbrella term referring to several different types of midwives. There is a CNM- certified nurse midwife, a certified midwife, and a lay midwife. There are training differences for each of these types of midwives and the only ones that can work in a hospital setting are CNM’s. There are strict state/medical/nurse midwife/hospital board guidelines that dictate the scope of hospital-based practice. I am not sure why a person would choose the different routes, but I am sure that the cost and duration of training are huge factors.
Can you discuss how beneficial it has been to have midwives as part of your practice and how what they might bring to the birthing experience differs from what an OB might bring? And perhaps how having the two together – midwives + OBs – proves most beneficial to patient care?
It is actually a little hard to answer this question because I don’t think of the practice as an OBGYN practice that has midwives but rather a collaborative practice. Therefore, the benefit of having CNM’s in the practice is that our patients truly get the best type of care. CNM’s appointments are longer, although not by much, some patients get one CNM for the entire antepartum care while most others see a fair share of our CNMs. I think this is helpful as there is a familiarity with the CNM attending your triage calls, L&D triage visits, and delivery. In the clinic setting, patients benefit visits like a “spiritual cesarean” and other wisdom from Birthing From Within as some of our CNMs are also Birthing From Within educators. In the hospital setting, peanut balls, robozo techniques, and other Spinning Babies expertise to help rotate babies.
At the discharge, CNMs spend a great deal of time going over common questions, follow up precautions, and of course breastfeeding is highly encouraged and there are hospital based lactation consultants. In case of clinical concerns, the OBGYNs are a phone call away and each high-risk patient is discussed in a weekly case conference for management collaboration. In the hospital setting, if an emergency or complication arises, which needs immediate attention, the OBGYN’s are again a phone call away. Truly, the collaborative models are an incredible resource that puts the patient and her pregnancy and birth experience at the forefront of the practice.
How do you balance the defense of the obstetrics profession with your empathy for those individuals who, like myself, have less than ideal things to say about their own experience with their practitioner?
I welcome opportunities like this to educate and communicate. The professions have become so segregated but ultimately the end goal is a happy healthy couplet. We can’t loose sight of this in the name calling game.
One of my friend’s husbands is an OB and he says he is very bothered by the birthing-at-home trend. He said, “Birth either goes totally fine or there are major complications requiring a hospital setting. There’s rarely an in-between.” What are your thoughts on this?
I would agree. That is why sticking to strict guidelines for eligibility of a home birth is so important.
These guidelines were created to ensure a level of safety in a risky situation. Our bodies and our births are unpredictable.
Do you find that the location of an OB practice matters? It seems that in very busy metropolitan areas, the staff is so overbooked and stressed, so even if the doctors have good intentions, they simply don’t have the time for personalized care.
I don’t think I can fairly answer this. I will say that the example you pose would argue completely against the UCSD model- a hospital based birthing center inside a metropolitan academic institution. I don’t think the location of an OB practice is so much the issue but the administration and staffing support of the hospital.
I have a friend who recently birth her fifth baby and for the first time was told she needed to put her legs in stirrups. Can you touch on how different hospitals have different practices and how somethings might be allowed at one hospital but aren’t at others?
I encountered this myself the other day at a birth. Typically the people helping a woman push for 1-3 hours is a loving family member and the labor and delivery nurse. This nurse wears multiple hats during this second stage of labor. Having her be responsible for leg holding takes her focus off fetal monitoring, vitals monitoring, and overall lay of the LDR. Therefore, if no other family member is available to help with leg holding, especially in an anesthetized birth, where the leg is really heavy, then stirrups are used. The growing trend of rise in BMI’s also feeds this answer. It is something that is worth addressing but women with higher BMI’s have a higher risk for pregnancy complications and in the second stage require a greater level of nursing support.
As far as differences in hospital delivery practices it comes down to the administration as well as the attitude/culture of the OBGYN Division in that particular hospital. We are all governed by ACOG, American College of Obstetrics and Gynecology. However, there are variances within and different degrees of confidence/training/expertise amongst the staff in each L&D setting. For example, an assisted vaginal delivery can be either via a vacuum or by forceps. If the department has OBGYN’s who were trained in either technique more than the other, then you will see a shift in assisted vaginal delivery techniques. The culture of our training sites has so much to do with how OBGYN’s practice as well. For example, in my residency we used cytotec, misoprostol as an induction agent. However, in my current practice, everyone was using cervidil and so I had to adjust my level of comfort with in.
How much of a role does the hospital have on the dictation of care a physician renders?
A LOT. A silly example would be how much of a role does the HOA of a condo complex have when you rent out the community area and pool. Ultimately, the HOA is also liable in any adverse events.
Therefore, the hospital administration, nursing administration and along with the division of OBGYN staff, together dictate the guidelines. Protocols are written by, reviewed, and agreed upon by all involved.
I’ve often gotten the sense that the majority of OBs are most comfortable when delivering a baby in bed. Is this due to the way OB’s are taught / trained? Why is there trepidation with allowing a woman to labor and birth a baby in water? Water is a wonderful pain reliever for those who chose to go the natural route but it is rarely allowed in the hospital setting (outside of showers, which don’t really offer the same great relief as a birthing tub). Can you discuss this? And how does your practice navigate around the hospital limitations?
You are correct. I am not aware of any OBGYN residency that offers training in water births. The typical delivery position we are trained in is supine/semi fowlers. However, those residents who have the fortune of having CNMs in their training institutions may have experience and comfort with other delivering positions. It is unfortunate that the OBGYN is finger pointed as the bottleneck for water births when there are so many layers to consider. These have to do with infection control, staffing, resources/equipment, and the rate of turnover (house keeping). There needs to be buy in from all these departments including Administration (finances, maintenance, engineering), Infection Control, RN, and Housekeeping in order to keep a water based practice practical and safe.
As one of my CNM mentors asked me in discussing this answer, “do you like cleaning your own tub at home?”
Now imagine this with industrial strength chemicals, several times a week.
The number of c-sections performed has gone up dramatically (only now starting to go down a bit). Do you think this is because of fear of liability issues? Or insurance payouts? Or convenience for all parties? Or all of the above?
There are many factors to this beyond what you have listed here. First, you need to consider the change in the body habitus of women. We are seeing a lot more obesity and women with BMI > 35 having children. In addition to underlying obesity, the associated medical conditions such as diabetes, PCOS, and liver disease certainly affects the health of the pregnancy. Babies of diabetic mothers are bigger and certainly at higher risk for birth trauma and therefore warrant evaluation and discussion for a primary cesarean section. The second overlooked factor is general living condition of pregnant women. Our society has become one of “deep couch sitting” and screen time. This reclined posture found in cars, theaters, at home, etc. perpetuates an occiput posterior (OP) position for the fetus. In the OP position, the largest portion of the fetal vertex needs to engage the pelvic bones hence making labor more painful and longer. The insurance payout, convenience statement might be true for some “bad apples” but it is certainly not for the majority of OBGYNs. Fear of liability is better understood as a fear of bad outcome for either the mom or the baby. OBGYNs have the lives of 2 people on their hands and it is the high desire for a good outcome along with the litigation scares that may sway decisions. The invention of fetal heart rate monitoring has contributed to the overall higher number of cesareans. Now we have a tracing that indicates what the fetus is experiencing and OBGYN’s are going to act to rectify the intrauterine environment, which may mean a cesarean section.
I read recently that “because birth matters. How you give birth matters.” This was a very well done article on thebestofbaby.com. For the most part I agree. It does matter if your arms are tied down to the operating table, if your legs are in stirrups, if you are on your back, or upright in a tub, or squatting on a ball. The entire birth experience matters as it becomes your babies story and how you both exist as a couplet now. In order to have your birth experience, I encourage women to speak up, ASK questions, TALK to your physician. There is no way that you will get your birth experience if you haven’t communicated and understood the practices of your physician. Brining in a doula is essentially giving your power to someone else, someone who is paid to be your advocate. But you can be your own advocate from the beginning.
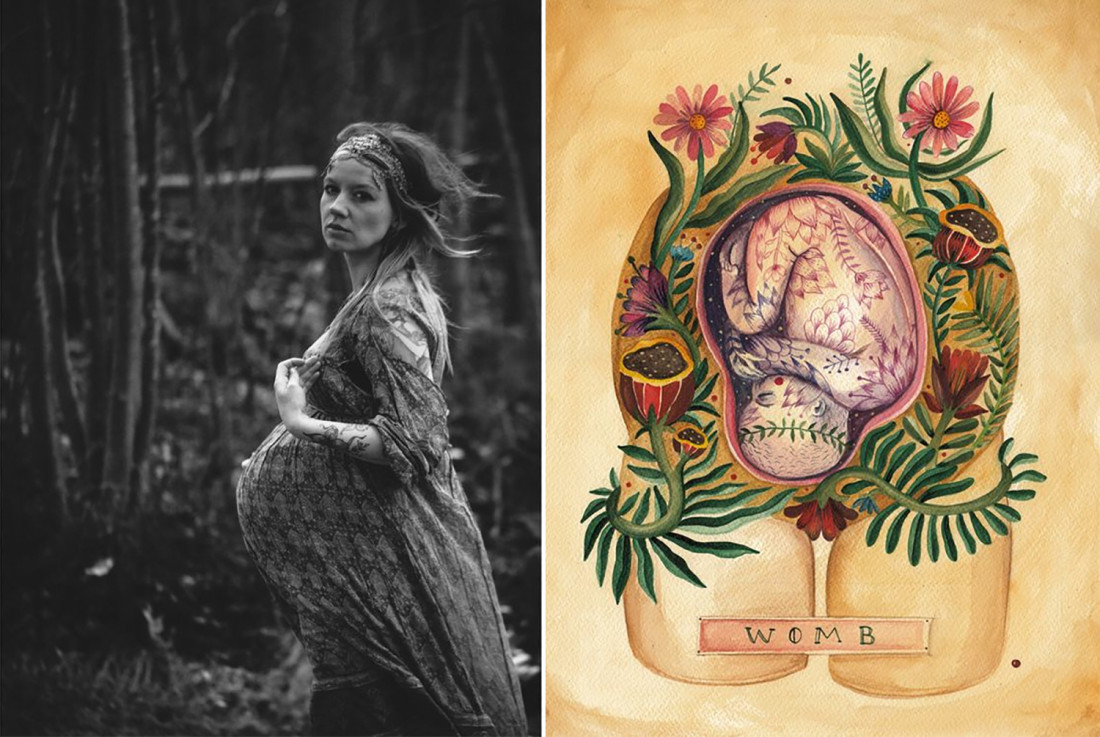
Image of pregnant woman by By Rosenoff | Birth art found on Pinterest
Thanks for this! As you know, I’m a huge advocate of the midwife and the birth center experience, but I LOVE the way the conversation and education around birth is expanding and I love that there are options for women that aren’t so polarized. This was a great middle-ground perspective.
Really great interview! I experienced a little bit of both sides, and I really do hope that more of a middle ground can be found for more women. There is a great benefit when OBGYNs and Midwives can work together. It’s definitely interesting to hear the perspective of a doctor.
I personally prefer the midwifery model of care. That being said, as this interview points out there are several types of midwives. In my opinion a CNM is the most versatile and they are allowed to practice in a hospital setting. You want to find out the stats for your midwife and if you’re planning a home birth, you’d want to know what their transfer rate is and what the reasons for transfer were.
I did choose a midwifery practice that only did hospital births. They are closely affiliated with an OBGYN practice that they often refer to. If you are deemed a high risk pregnancy or birth, the midwives won’t care for you but the OB practice does. Just as if an emergency happens during the labor and birth that requires a cesarean, one of the physicians steps in and takes over.
Thanks for this post! Her practice would be my ideal model for prenatal care. It’s too bad such a practice does not exist in my state.
Amazing post and Thank You!!! I am one of the lucky CNMs that works with Ema!! We are so lucky to have her and 4 other fabulous OBs that we collaborate with. She is such a blessing to our practice!!
Thank you again for this interview:-)
Oh so awesome to know that others that work with her are into reading the interview as well. Thank you, for all you do.
Thank you for this! Great read.
I dislike her comment regarding doulas!!! One service a doula performs is to provide education so women can advocate for themselves. A doula should not be advocating for a client. But this is also just one facet of a hugely dedicated and deep job!! Her comment diminishes it greatly. Ugh, *facepalm*
I see your point. Perhaps what she meant is that we’re all capable and free to educate and advocate for ourselves?… but as someone who has given birth naturally twice, words aren’t easy to form and it was really nice to have someone there that knew how to navigate the hospital system and speak on my behalf AND support my husband. I agree that doulas are priceless.